Liver

Your liver looks like a blood-filled, three-pound sponge wedged between your ribs. If you observed its function, however, it would resemble a metabolic processing plant with specialized sorting centers where vital nutrients are stored and dangerous toxins are filtered out – every three minutes.
Your biggest, most regenerative organ processes and stores proteins, carbohydrates and nutrients, so your blood can deliver them to the organs in need. It also creates blood clotting factors to help you stop bleeding after an injury.
Unlike your kidney, gallbladder, spleen, or appendix, you cannot live without your liver. Transplants are difficult, painful, and life-altering. Donated organs are hard to come by. Protecting and nurturing this vital organ is imperative – and because it’s the most resilient and regenerative solid organ in your body, there are many ways to do so.
Liver functions
Your liver consists of two lobes (a larger right lobe and a smaller left lobe) that perform over 500 essential tasks, including:
- storing sugar as glycogen and converting it back when you need energy
- creating blood clotting factors
- creating amino acids, including those that help fight infections
- processing and storing iron necessary for red blood cell production
- creating and metabolizing fat, cholesterol, and carbohydrates
- turning waste products into urea in urine
- metabolizing medications into their active ingredients
- absorbing and metabolizing bilirubin (the byproduct of hemoglobin breakdown)
- creating angiotensinogen, a hormone that raises blood pressure
- creating albumin, a protein that transports fatty acids and steroid hormones to help maintain optimal pressure and prevent blood vessel leaking
- secreting bile, a greenish-brown alkaline fluid that aids in our digestion (which is why it’s also considered a gland)
The liver is the only visceral organ that has the capacity to regenerate after either injury or surgical removal. As little as 25% of your original liver mass can regrow back to its original size.
Preventing liver damage
How can you regenerate damage or avoid the many liver conditions that affect about 3.9 million Americans? By properly fueling and maintaining this amazing biochemical processing plant.
According to the American Liver Foundation, eating high-fat foods can stress your liver, compromise your immune system, and increase your risk of obesity. To avoid these issues:
- eat a diet low in saturated and no trans-fat
- avoid fried foods to prevent fat overload that can lead to nonalcoholic fatty liver disease
- eat lean protein like fish to rebuild and replace liver cells damaged by diseases like hepatitis C
- eat white chicken and skinless turkey meat, as these are high-protein but low-fat
- avoid high-sodium foods, which can cause water retention and inflammation, overburdening your liver
- limit high-fat red meat, which is harder for your liver to break down
- eat lots of fresh vegetables and fruits (organic if possible) for antioxidants and healthy fiber, which eliminate toxins from your body
- eat complex carbohydrates (whole grains and high fiber) to increase insulin sensitivity and lower your blood cholesterol
- drink 8-12 eight ounces of filtered water daily, as 73% of your liver is water
- refuse processed foods – stick with fresh or frozen to cut back on salt
- reduce sugar, because your liver turns the sugar fructose into fat; too much sugar can cause fatty build-up, leading to fatty liver disease
- limit alcohol (which turns into sugar)
- enjoy low fat or non-fat dairy products, as these are high in whey protein that may protect your liver from further damage
If you simultaneously practice these lifestyle choices, this diet will help you maintain a healthy weight and keep your liver smoothly humming along:
- avoid smoking
- avoid illegal drugs
- avoid pharmaceutical medications that list liver damage as a side effect (see below)
- manage diabetes effectively
- exercise for at least 30 minutes each day
- avoid contact with other people’s blood and bodily fluids
- do not share needles, razors, toothbrushes, nail care tools, or pierced earrings
- use condoms
- cover all open cuts and wounds
- don’t share chewing gum or pre-chew food for a baby
- get the hepatitis A and hepatitis B vaccines
- wear gloves, long sleeves, a hat, and a mask when spraying insecticides, fungicides, paint, and other toxic chemicals; when painting make sure the room is well-ventilated
Causes of liver damage
Liver disease (hepatic disease) is any kind of disturbance of liver function that causes illness. Usually, more than 75% of the liver must be affected before function is impaired.
Like most health disorders, liver disease is caused by multiple synergistic agents – both biological (genetics, hormones) and environmental (viruses, ingested chemicals, environmental toxins).
Pharmaceuticals and chemicals
The most common culprits of chemically-caused liver disease include:
- aspirin
- antibiotic steroids
- excess amounts of acetaminophen (Tylenol, Panadol) and nonsteroidal anti-inflammatories (NSAIDs) like ibuprofen (Advil, Motrin IB)
- prescription narcotic-acetaminophen combination medications (Vicodin, Lortab, Norco)
- drugs prescribed to control elevated blood levels of cholesterol (statins and niacin)
- antibiotics like nitrofurantoin (Macrodantin, Furadantin), amoxicillin and clavulanic acid (Augmentin, Augmentin XR), tetracycline (Sumycin), and isoniazid (INH, Laniazid)
- methotrexate and disulfiram
- oral contraceptives (birth control pills)
- certain antiepileptic, antifungal, antipsychotic, and antimicrobial drugs
- mnemonics like Paracetamol
- toxic chemicals like vinyl chloride and carbon tetrachloride
Viruses
The most common causes of viral hepatitis are the five unrelated hepatotropic viruses hepatitis A, B, C, D, and E. They can be contracted through exchange of bodily fluids, use of IV drugs or needle-sharing, and unsanitary living conditions.
In some infected people, the virus remains dormant, and they do not develop acute illness. A synergy of genetic, hormonal, immune system and environmental factors can activate it.
Bacteria
Most bacterial infections in the liver cause secondary hepatitis with unique clinical features. Bacteria from a ruptured appendix causes pyogenic liver abscess infection. Multiple bacteria are to blame in 50% of these abscesses. Infection from a slew of mycobacteria species can cause chronic or granulomatous hepatitis.
Hormonal imbalance
Autoimmune hepatitis is often triggered by certain anesthetics and antibiotics that alter liver proteins, causing your body to mistake its own liver cells for foreign invaders. But it’s the hormone estrogen that colludes with a signaling molecule (interleukin-6) to drive the immune cell misconduct that fuels liver damage.
That’s why this form of hepatitis is more common in women. Altering the estrogen-to-testosterone ratio may hold the key to staving off liver degeneration.
The hepatitis B virus that can lead to liver cancer is more common in males and postmenopausal females. Increasing evidence suggests that androgens and estrogens may trigger the progression of these diseases.9 Deficiencies of the DHEA hormone have also been implicated in hepatitis progression.
Because auto-immune hepatitis does not present with the same symptoms as other forms make it’s difficult to diagnose. Often diagnosis requires a biopsy.
Genetic abnormalities
Some genetic conditions cause substances to build up in the liver:
- Gilbert’s syndrome: a bilirubin metabolism abnormality
- hemochromatosis: abnormal iron levels that cause inflammation, cirrhosis, liver cancer, and liver failure
- Wilson’s disease: improper copper metabolization that may lead to cirrhosis and liver failure
- alpha-1 antitrypsin deficiency: low levels of a protein called alpha-1 antitrypsin (A1AT)
- alagille syndrome: malformed bile ducts cause bile build-up and liver scaring
- lysosomal acid lipase deficiency (LAL-D): a rare, chronic, progressive disorder that disrupts production of lysosomal acid lipase, which breaks down fats and cholesterol
- glycogen storage disease type 1 (von Gierke): glucose buildup impairs function
- cholestasis and gallstones : sometimes caused by pregnancy
- Budd Chiari syndrome: an abnormally elevated red blood cell count can cause inflammatory bowel disease and sickle cell disease, clotting blood in the hepatic vein and preventing it from leaving the liver
- benign tumors: abnormal cell growths in the liver
- hepatic encephalopathy: increased ammonia levels caused by the liver's inability to process and metabolize proteins can cause confusion, lethargy, and coma
- abnormal bleeding: decreased liver function can reduce the blood-clotting factors in your body and increase your risk of bleeding
- lack of protein creation: affects various bodily functions
- portal hypertension: increased blood vessel pressure in the liver can affect blood flow to other organs, causing swelling in the spleen and esophagus
Symptoms of liver damage
Generally, liver damage presents abdominal pain, along with stomach upsets like nausea, vomiting, diarrhea, and pale, bloody, or tarry-looking stool. Jaundice (yellowing of your eyes and skin) is also a common symptom. You may feel chronic fatigue, muscle weakness, joint pain, loss of appetite, swelling in your abdomen or legs, and mysterious weight loss.
Signs of liver problems like liver damage can be generalized and mimic those of many other medical conditions. Consult your healthcare provider so liver conditions can be ruled out or diagnosed.
A liver condition that affects your brain—like Reye's syndrome and hepatic encephalopathy—can cause confusion, irritability, hallucinations, personality changes, and seizures. These conditions can be life-threatening, so if you’re experiencing them, don’t wait—call 911 or get emergency medical attention right away.
Liver conditions
The most common liver conditions are hepatitis, cirrhosis, fatty liver disease, Epstein-Barr virus (EBV) infection—usually called mononucleosis, or just mono—and liver cancer.
Hepatitis
Hepatitis is liver inflammation caused by viral infections, toxins like alcohol, certain classes of pharmaceuticals, hormonal imbalances, and autoimmune dysfunctions.
The five infectious types of hepatitis are:
- hepatitis A (HAV): this acute, self-limiting condition is commonly spread by contaminated food or water; 4,000 cases are diagnosed each year
- hepatitis B (HBV): caused by contact with infectious body fluids like blood, vaginal secretions, or semen – drug injection, unprotected sex, and shared razors can increase infection risk; affects 800,000 – 2.2 million people in the U.S.
- hepatitis C (HCV): one of the most common types; transmitted through infected body fluids, via drug injection, unprotected sex, or blood transfusion; about three million people in the US live with chronic hepatitis C
- hepatitis D (HDV or delta hepatitis): a rare and serious virus caused by direct blood contact that only occurs in conjunction with HBV
- hepatitis E (HEV): a rare waterborne virus mainly found in areas with poor sanitation
- hepatitis G (HGV or GBV-C): caused by a single-stranded RNA virus, this recently-discovered virus is almost always asymptomatic – requires more research
Non-infectious hepatitis types are:
- alcoholic hepatitis : caused by excessive alcohol consumption
- autoimmune hepatitis : genetic factors, hormone imbalances (like DHEA deficiency or excessive estrogen) that increase antibodies, or pharmaceutical drugs can cause your immune system to attack your liver
Hepatitis treatments
As with any medical procedure, results of liver disease treatments will vary from patient to patient depending on age, genetics, general health, condition severity, follow-up care, and environmental factors.
The following pharmaceutical, regenerative, nutritional, and botanical treatments may present contraindications with one another, and/or with other medical conditions. Consult your healthcare provider before embarking on your treatment journey.
Nutritional and supplemental treatment for hepatitis
Excessive alcohol and foods that raise insulin levels damage your liver. To maintain healthy liver function avoid:
- sports drinks, soda, energy drinks, and juice: contain sugar that can cause fatty liver disease
- hydrogenated oils, refined sugar, convenience foods: these processed foods are filled with high fructose corn syrup, a major cause of non-alcoholic fatty liver disease8
- white bread, white rice, and corn: these refined carbohydrates raise insulin levels and increase the risk of liver disease
The complete cessation of alcohol consumption leads to a regression of fat deposits between tissues within four to six weeks.4
Foods that can detox your liver include kale, cabbage, cauliflower, broccoli, Brussels sprouts, asparagus, beets, celery, sweet potatoes, and bananas.
Clinical trials have shown that the following supplements can address liver damage:
- intravenous (IV) therapy: intravenous infusion delivers high concentrations of vitamins and minerals directly into your bloodstream; intravenous vitamin C has been shown to have anti-tumor and anti-hepatitis effects
- antioxidative therapy: studies show that a combination of intravenous and oral antioxidants benefit patients with chronic HCV infection who don’t respond to interferon.1
- N-Acetyl cysteine (NAC): replenishes glutathione, which neutralizes the toxic metabolite in acetaminophen (the most common cause of acute liver failure)
- vitamin E: a cell membrane antioxidant that reduces inflammation; shown to produce significant liver tissue improvements in biopsies
- vitamin B12: research shows that adding this vitamin to interferon treatment clears the hepatitis C virus
- alpha-lipoic acid: this powerful antioxidant has been shown to decrease the amount of hepatic fibrosis, and to enhance the effects of other antioxidants
- pyruvate dehydrogenase kinase (PDK): this mitochondrial enzyme promotes the breakdown of glucose molecules (aerobic glycolysis)
To learn more visit our Nutritional and Supplement Treatment for Hepatitis page.
Pharmaceutical treatments for hepatitis
Medications can be prescribed alone or as part of a larger treatment plan. The most commonly prescribed pharmaceutical treatments for hepatitis C—pegylated interferon alpha and ribavirin—have a 50% success rate and present side effects in 80% of patients.
To avoid the serious side effects of interferons, researchers developed Direct-Acting Antivirals (DAAs) to target RNA proteins and enzymes and prevent replication of the hepatitis virus. Preliminary trials show promising results and less adverse side effects.
These medications should always be taken exactly as directed and under your provider’s careful monitoring:
- lactose: this sugar can induce bowel movements to excrete toxins like ammonia
- diuretics: decrease intracranial pressure and increase urination
- kanuma enzyme replacement: treats LAL deficiency
- prednisone: lowers immune system activity
- azathioprine: suppresses immune system activity
- intravenous (IV) glucose and electrolyte solution: treats low blood sugar or water loss without electrolyte loss
- ursodeoxycholic acid: decreases bile acids in cholestasis of pregnancy
Studies on liver cirrhosis patients show that 20% of the drugs prescribed are dosed incorrectly, and almost 30% of patients with cirrhosis suffer adverse drug reactions.6
Hepatitis A and B vaccines are recommended if you:
- are a healthcare worker
- work in a daycare center, school, or jail
- are traveling to an area where infections rates are high
- come into contact with infected blood or body fluids of friends or family members
- are a man having sex with other men
- have a blood-clotting issue
- use needles to inject illegal drugs
- have a long-term liver disease
To learn more, visit our Pharmaceutical Treatments for Hepatitis page.
Botanical medicine for hepatitis
Botanicals – medicinal substances obtained from plants – can biochemically correct enzyme and hormone imbalances in the liver. Studies have shown that silymarin (milk thistle) detoxifies the liver by protecting its cells from some forms of free radical damage, and is well tolerated in chronic HCV-infected patients.7
Other evidence-based, time-tested botanical treatments include:
- dandelion root: has the ability to increase the flow of bile, and reduce water weight
- black seed oil: shown to significantly reduce HCV viral load, oxidative stress, and edema
- licorice root: contains anti-inflammatory anti-oxidant glycyrrhizin
- bupleurum: contains anti-inflammatory substances called saikosaponins
- cordyceps: this antioxidant stimulates the immune system of cirrhosis and hepatitis patients
Learn more on our Medicinal Botanicals for Hepatitis page.
Acupuncture therapy for hepatitis
To treat chronic enzyme and hormone imbalances that can over-activate the immune system, acupuncturists stimulate meridians along your interstitium to increase blood flow and rebalance enzyme and hormone levels in your liver.
Acupuncture treats imbalances by:
- increasing blood flow and red blood cell creation in liver tissue
- regulating glucagon and insulin hormone levels to balance blood glucose level
- releasing neuropeptides
- sending inflammatory proteins and white blood cells to damaged tissue
- eliminating toxins
Learn more on our Acupuncture Therapy for Hepatitis page.
Stem cell therapy for hepatitis
Liver diseases like cirrhosis of the liver and hepatitis can be treated with stem cell therapy. Stem cells are specialized cells in your body that have the ability to stimulate your own damaged cells to regenerate, strengthening your tissues.
Specifically, regenerative therapies using functional hepatocyte-like cells derived from pluripotent stem cells may be able to treat liver diseases.2
Learn more on out Stem Cell Therapy for Hepatitis page.
Surgical procedures
Surgery can remove damaged liver tissues. Benign liver tumors can be surgically removed if they cause pain or bleeding. Patients with gallstones may require gallbladder removal.
Fluid in ascites is removed with a needle and syringe (paracentesis). This increases your risk of spreading bacteria to cause brain abscess, eye infection that can lead to vision loss, or lung artery clotting. Surgery is also done to treat portal hypertension.
Part of your liver (partial hepatectomy) can be removed to treat cancer. In cases of liver failure, a liver transplant can replace your liver with either an entire liver from a recently-deceased person or part of a living person’s liver. More than 5,000 liver transplants are performed in the United States each year.5
To treat A1AD, shunts may be inserted to lower the pressure within the blood vessels in the liver and dilated esophageal veins may be clipped or banded to lower the risk of bleeding.
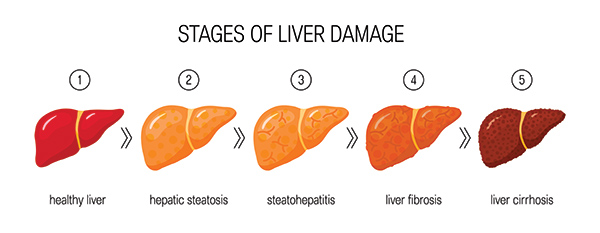
Cirrhosis
Cirrhosis is late stage scarring of the liver usually caused by hepatitis and alcohol abuse. Cirrhosis can cause jaundice, fatigue, easy bruising and bleeding, nausea, male breast enlargement and testicular atrophy, itchy skin, mysterious weight loss, confusion, and slurred speech.
Cirrhosis can’t be reversed. This permanent scarring blocks blood flow in and out of the liver. At this stage, providers can only minimize further damage and manage symptoms.
Fatty liver disease
Fatty liver disease or hepatic steatosis is the buildup of fat in the liver. Excessive liver fat can cause dysfunction and symptoms like low appetite, weight loss, abdominal pain, and fatigue.
There are four types of fatty liver disease:
- non-alcoholic fatty liver disease (NAFLD): not related to alcohol; develops when the liver has difficulty breaking down fats, which causes a buildup in the liver tissue; diagnosed when more than 5% of your liver is fat
- non-alcoholic steatohepatitis (NASH): a type of NAFLD diagnosed when your liver fat content is higher than 5% and inflammation as a result of fat buildup is present
- acute fatty liver of pregnancy: can occur during your third trimester and can be life-threatening; once symptoms are managed it typically resolves and causes no long-lasting complications
- alcoholic fatty liver (AFL): occurs because heavy drinking damages your liver and impairs its ability to process fats; AFL is the earliest stage of alcohol-related liver disease and is typically caused by heavy long-term drinking; usually resolves when you stop drinking and your liver has time to process out the built-up fat; if you don’t stop drinking, alcoholic steatohepatitis can result, eventually causing cirrhosis
Epstein-Barr virus (EBV)
Commonly called mono and human herpesvirus 4, EPV is one of the most common human viruses. It’s spread through human bodily fluids like saliva, blood, or semen, blood transfusions, and organ transplants. The Centers for Disease Control (CDC) reports that about 95% of people in the US have been infected at some point in their lives, typically between the ages of 15-17.
Liver cancer
Liver cancer begins in your liver cells. When factors cause these cells to mutate and reproduce, they can form into tumors, which then cause cancer.
There are several types of liver cancer. These include:
- hepatocellular carcinoma: begins in the most common type of liver cell (hepatocyte), and is the most common
- intrahepatic cholangiocarcinoma: the second most common type originates in your peripheral bile ducts; is very uncommon
- hepatoblastoma: a very rare tumor typically caused by genetic factors; mostly affects children from infancy up to three years of age
Treatments for liver cancer include:
- radiation: high-energy rays can kill your cancer cells; radioactive particles are injected into your artery to block or destroy the blood supply to your liver tumor (internal)
- chemotherapy: your physician puts a thin, flexible tube into your artery to deliver chemotherapy drugs (mixed with another drug) to your liver to kill the tumor by starving it of blood
- alcohol injection (percutaneous ethanol injection): your physician injects alcohol (ethanol) into your liver using an ultrasound while you’re under anesthesia
- cryoablation: your physician destroys the tumor by freezing it with a metal probe while you’re under anesthesia
- radiofrequency ablation: similar to cryoablation, it instead uses an electric current
It has been suggested that radiofrequency ablation (RFA) leads to better overall survival in patients with operable HCC than in those with inoperable HCC.3
Diagnosing liver conditions
Blood tests are an important way to assess liver inflammation and function. A liver function panel is a group of tests that detect a variety of biomarkers:
- alanine aminotransferase (ALT): elevated ALT helps identify liver disease or damage from conditions like hepatitis
- GGT and alkaline phosphatase (chemicals released by cells lining the bile ducts)
- bilirubin: high levels indicated liver imbalance
- complete blood count (CBC): this looks for low red blood cells, white blood cells, and platelets in patients with end-stage liver disease and cirrhosis
- INR blood clotting function: this may be impaired due to poor protein production
- ammonia blood level assessment: used for patients with mental confusion to determine if liver failure is responsible
- protein and albumin: this helps determine how well your liver is working
- viral hepatitis: these tests check for hepatitis A, B, and C
- prothrombin time and partial prothrombin time: this is commonly done to see if you’re taking the correct dose of warfarin, and to check for blood clotting issues
- fasting blood sugar: this test is taken after an overnight fast
- hemoglobin A1C: this shows how stable your blood sugar is
- lipid profile: this measure blood fats like cholesterol and triglycerides
- TCM diagnosis: tongue, pulse, and facial analysis to determine which acupuncture meridians require stimulation
- liver scan: this scan uses radioactive material to help diagnose abscesses and tumors
- liver biopsy: microscopic analysis of extracted tissue
- imaging tests: an ultrasound, CT scan, and MRI can reveal liver damage from cirrhosis, and conditions like gallstones
- transient elastography: an enhanced ultrasound that measures the stiffness of your liver (liver stiffness indicates cirrhosis)
- magnetic resonance elastography: this combines magnetic resonance imaging with sound waves to create a map of the liver
- spinal tap (lumbar puncture): collects cerebrospinal fluid for lab analysis via a needle inserted through your spine to diagnose Reye’s syndrome
Learn More Today
The liver is an amazing organ that keeps your body toxin-free. That’s why it’s important to take care of yours. There are many treatments available to help you heal any liver damage caused by lifestyle choices, hormone imbalances, or viruses. To learn more about preventing and treating the liver visit our Vitadox condition and treatment pages.
Sources:
- A, Melhem, et. al. “Treatment of chronic hepatitis C virus infection via antioxidants: results of a phase I clinical trial.” Journal of Clinical Gastroenterology 39.8 (2005): 737-742. Web. 21 August 2018.
- Horisawa, Kenichi, and Atsushi Suzuki. “Cell-Based Regenerative Therapy for Liver Disease.” Innovative Medicine: 327-339. Web. 21 August 2018.
- Lin, Shibo, Katrin Hoffmann, and Peter Schemmer. “Treatment of Hepatocellular Carcinoma: A Systematic Review.” Liver Cancer 1.3-4 (2012): 144–158. PMC. Web. 21 Aug. 2018.
- Sevastianos, Vassilios A, and Spyros P Dourakis. “Alcoholic Liver Disease: A Clinical Review.” Journal of Nutrition & Food Sciences (2016). Web. 21 Aug. 2018.
- Siddiqui, Aliya, et. al. “Stem Cell Therapy for Liver Diseases.” Journal of Stem Cell Research & Therapy (2011). Web. 21 August 2018.
- Weersink, Rianne A, et. al. “Evaluating the safety and dosing of drugs in patients with liver cirrhosis by literature review and expert opinion.” BMJ Journals 6.10. Web. 21 August, 2018.
- Z, Yang, et. al. “Effects and tolerance of silymarin (milk thistle) in chronic hepatitis C virus infection patients: a meta-analysis of randomized controlled trials.” BioMed research international (2014). Web. 21 August 2018.
- Basaranoglu, Metin, et al. “Carbohydrate Intake and Nonalcoholic Fatty Liver Disease: Fructose as a Weapon of Mass Destruction.” Hepatobiliary Surgery and Nutrition, Apr. 2015, pp. 109–116., doi: 10.3978/j.issn.2304-3881.2014.11.05.
- Maurizio Montella, Giovanni D'Arena, Anna Crispo, Mario Capunzo, Flavia Nocerino, Maria Grimaldi, Antonio Barbieri, Anna Maria D'Ursi. Role of Sex Hormones in the Development and Progression of Hepatitis B Virus-Associated Hepatocellular Carcinoma . Int J Endocrinol. 2015; 2015: 854530. Published online 2015 Sep 27.
Vibrant Health Naturopathic Medical Center
Address
3 Riverside DriveGreenland, NH 03840
(207) 536-9661
www.vibranthealthnaturalmedicine.com
Hours
Mon:
8:30 am - 5:00 pm
Tue:
9:00 am - 5:00 pm
Wed:
10:30 am - 5:00 pm
Thu:
9:00 am - 5:00 pm
Fri:
10:00 am - 4:00 pm
Sat:
Closed
Sun:
Closed

